Abstract
An emerging theme among clonal hematopoiesis (CH) associated mutations is that these mutations endow hematopoietic stem cells (HSC) protection from chronic inflammatory stress. Specific inflammatory stressors may select for specific mutants, such that presence of particular mutant clones could be leveraged as a biomarker to herald the presence of a specific stressor. JAK2 V617F clonal hematopoiesis is less common among the general aging population but clusters within families suggesting that a specific stressor present among members of myeloproliferative neoplasm (MPN) families selects for JAK2 V617F mutant cells. We have recently found that monocytes from MPN patients and their unaffected family members have defective negative regulation of Toll Like Receptor Ligand (TLR) signaling due to a dampened response to the anti-inflammatory cytokine Interleukin-10 (IL-10) which leads to persistent TLR signaling and increased TNF production.
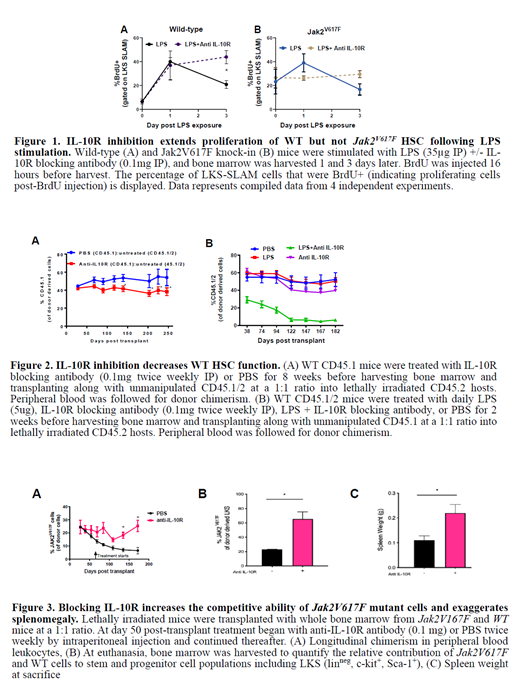
We hypothesized that IL-10 serves to curtail TLR signaling in HSCs just as it does in monocytes. Therefore, we assessed activation and proliferation of HSCs in WT mice treated with the TLR agonist lipopolysaccharide (LPS) versus mice treated with LPS + IL-10 receptor (IL-10R) blocking antibody (Fig 1A). As expected, LPS treatment induced proliferation of HSCs at day 1 which returned to dormancy by day 3. However, with IL-10R blockade, WT HSCs remained highly active and proliferative even at 3 days post stimulation (Fig 1A). In contrast, blockade of IL-10R in Jak2 V617F HSC did not extend the time period that HSC were actively proliferating post-LPS stimulation (Fig 1B).
To assess how chronic inhibition of IL-10R signaling impacts HSC fitness, we treated WT mice with twice weekly IL-10R blocking antibody and after 8 weeks harvested bone marrow for use in competitive repopulation assays. Bone marrow from mice exposed to chronic IL-10R blockade was inferior to untreated bone marrow (Fig 2A). We next tested whether blockade of IL-10R results in a functional decline in HSC when exposed to a short course of LPS exposure which would not otherwise result in defective competitive potential. We treated mice with 2 weeks of LPS +/- IL-10R blocking antibody before harvesting bone marrow for competitive repopulation assays. Whereas bone marrow from mice treated with 2 weeks of LPS competed equivalently to unexposed bone marrow, bone marrow from mice treated with 2 weeks of LPS + IL-10R blocking antibody were inferior to bone marrow from unexposed mice (Fig 2B). This demonstrates that IL-10R blockade accelerates inflammation induced exhaustion of WT HSC.
Reasoning that blockade of IL-10R signaling may lead to an inflammatory state that allows for Jak2 V617F mutant cells to gain a selective advantage, we injected bone marrow mosaic mice twice weekly with IL-10R blocking antibody starting at 50 days post-transplant. We observed an increase in the chimerism of Jak2 V617F mutant cells in mice exposed to IL-10R blocking antibody as compared to mice exposed to PBS, both in peripheral blood (Fig 3A) as well as in the stem and progenitor cell compartment of the bone marrow (Fig 3B). Moreover, IL-10R blockade exaggerated the MPN phenotype, with increased spleen size (Fig 3C) and increased megakaryocytes in the bone marrow and spleen (data not shown).
Together, these data demonstrate that IL-10R blockade accelerates inflammation induced exhaustion of WT HSC, likely due to increased cycling. Jak2 V617F HSC are protected from this accelerated exhaustion of HSC from IL-10R blockade, allowing them to gain a selective advantage in the context of chronic inflammation when IL-10R is blocked.
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal